The AI platform for healthcare operations
Personalize the patient experience, automate the work, and empower staff to practice at top of license.
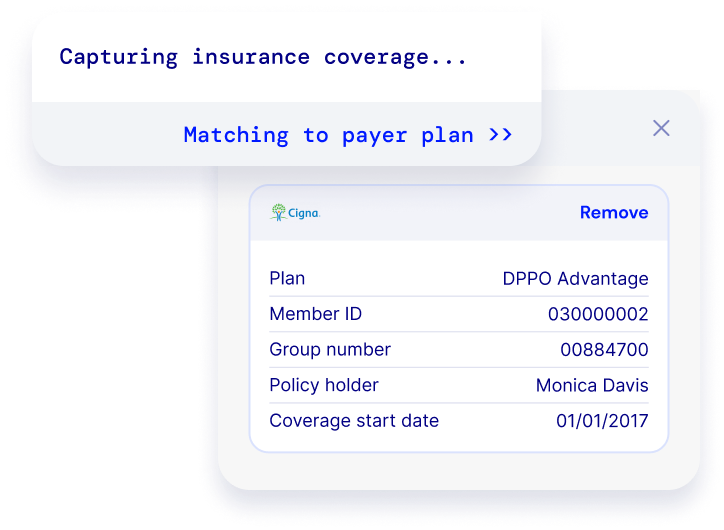

Build an intelligent digital front door
Personalize patient engagement with a unified experience across scheduling, appointment reminders, registration, intake, messaging and payments.

Build an intelligent digital front door
Personalize patient engagement with a unified experience across scheduling, appointment reminders, registration, intake, messaging and payments.
Optimize quality and risk management
Close more care gaps and improve VBC reimbursement by matching each patient to the care that they need.







Optimize quality and risk management
Close more care gaps and improve VBC reimbursement by matching each patient to the care that they need.
.png)




.png)
.png)
.png)
The Notable platform in action
Integration
Notable connects to your EHR and other systems, and our AI unlocks structured and unstructured data.
Automation
Notable’s AI performs manual workflows like patient outreach, EHR data entry, and document uploads just like human staff would.
Configuration
Business analysts and IT teams configure and customize workflows using a no-code interface.
Engagement
Notable powers personalized patient engagement across channels, including SMS, web app, patient portal, and your website.




Integration
Notable connects to your EHR and other systems, and our AI unlocks structured and unstructured data.


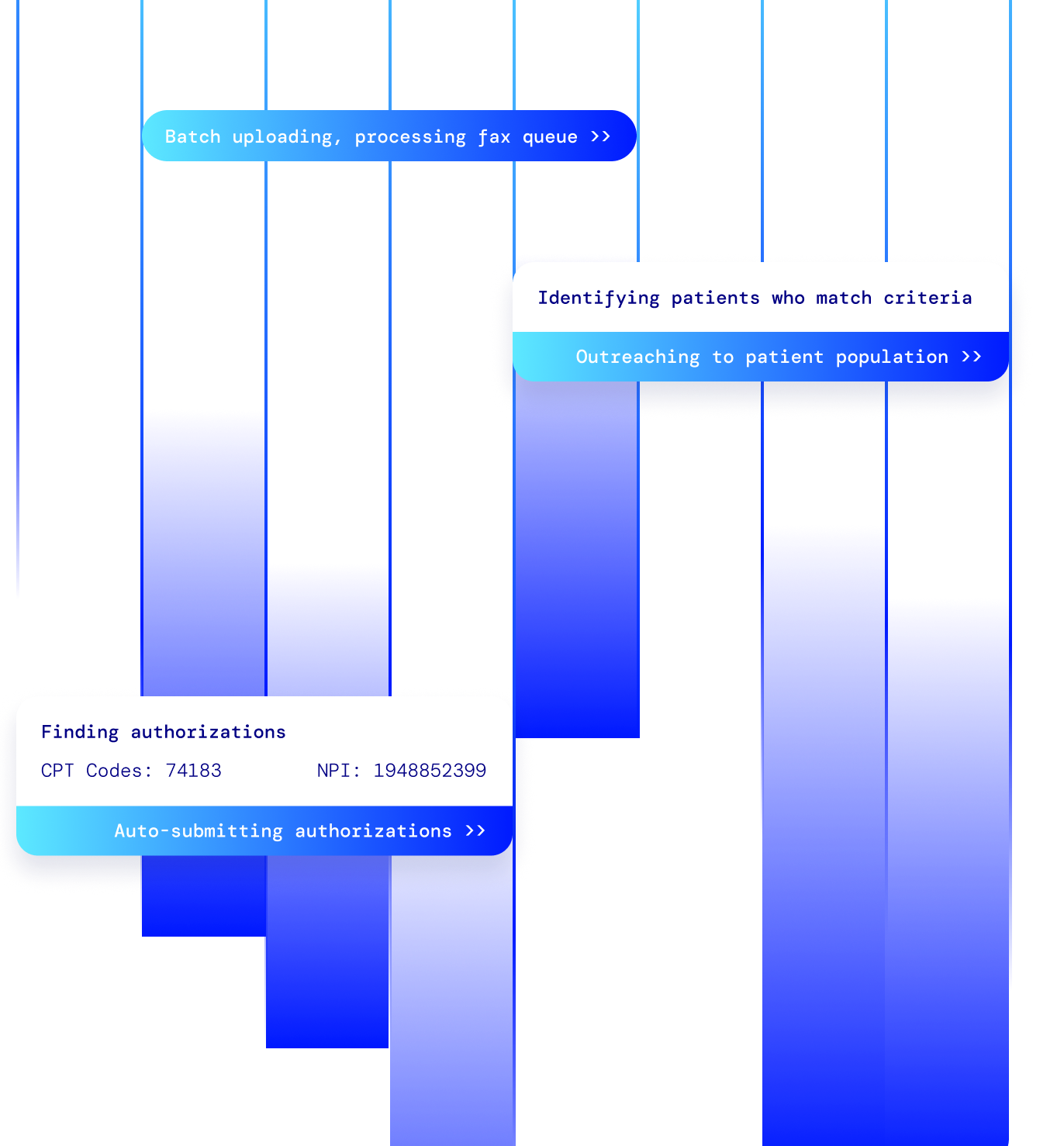
Automation
Notable’s AI performs manual workflows like patient outreach, EHR data entry, and document uploads just like human staff would.




Configuration
Business analysts and IT teams configure and customize workflows using a no-code interface.




Engagement
Notable powers personalized patient engagement across channels, including SMS, web app, patient portal, and your website.
How we partner
Notable drives demonstrable ROI for partners through Peak - our proprietary methodology for realizing financial outcomes from AI investments.

Assess baselines, define success criteria, determine scope, and align on success metrics.
Leverage best practice playbooks from other Notable partners to accelerate delivery.
Use agile delivery methodology to drive continual improvements in adoption and outcomes.
Assess hard and soft ROI realized from your investment in Notable.
Define new use cases for Notable’s AI, funded by value generated from existing implementations
Explore how others use Notable
reduction in check-in time per patient
open roles that didn't need to be filled
Digital front door
Cerner

How North Kansas City Hospital and Meritas Health automated 80 open roles
patient and caregiver satisfaction with Intake
patient satisfaction with Scheduling
Digital front door
Cerner
.png)
Gillette Children's offers world-class digital experience for complex care
reduction in no-shows
increased revenue capture within 3 months
Digital front door
Cerner

Good Shepherd Rehabilitation Network delivers best-in-class digital patient experience; reduces no-shows by 32%
pre-visit digital completion rate
patient satisfaction rating
Digital front door
Cerner

Intermountain Health drives 77% digital completion rate of well-child forms through automation
hours saved for registration staff over 6 weeks
success rate for insurance card capture
Digital front door
Epic

Montage Health drives over 200% increase in digital patient engagement within 6 weeks
touchless registrations
patient satisfaction rating
Digital front door
Epic

Austin Regional Clinic cuts documentation time by 50%
care gaps closed in 3 month period
estimated hours saved
Quality and risk
Epic


.svg)