The staffing shortage shows no signs of abating. High labor costs, burnout, and high turnover rates are impacting all roles across the health system, and the call center is no different. Despite hiring and retention challenges, phone-based scheduling remains the primary method for booking appointments in healthcare.
“Unfortunately, all roads still lead to the call center,” said Bri Buch, Head of Access Solutions at Notable. “That leads to a variety of points of friction that impact both the provider and the patient. Health systems are having to staff call center roles even as fewer and fewer adults are willing to pick up the phone, and patients can’t schedule appointments outside of business hours, which creates an obstacle to care.”
Why then, are health systems continuing to rely heavily on such an inefficient process for something as critical to the bottom line as scheduling?
- Summary
- Method
- Scheduling remains a highly manual, phone-based process
- Digital scheduling tools adoption
- The future of scheduling
Summary
Today's online scheduling options offload little burden; more than half of the respondents reported that less than 10% of visits are scheduled online.
Electronic health records (EHRs) are the dominant vendors, with 53% of respondents using their EHR’s native scheduling solution. However, a majority of providers express concerns about technical capabilities. Without the intelligence to personalize for both patient and provider, legacy solutions may be more limiting than liberating.
But automated scheduling matters for more than just efficiency — it can also be a competitive differentiator. As convenience grows in importance for patients, so too have digital capabilities. 75% of patients would like to complete any paperwork for their appointment ahead of time online, and 41% have switched providers due to a poor digital experience.
With so many patients invested in a digital, intuitive scheduling process, automated scheduling becomes essential to attracting new patients and retaining existing ones.
“We need to stop waiting by the phone for the right call center optimization measures. Patients will find the path of least resistance to schedule care,” said Susanne Katz, an Access Solutions Lead at Notable with prior experience managing the contact center for a large New York-based specialty hospital. “If others are offering that path with alternative and personalized ways to schedule, patients will take advantage of that convenience.”
No better time, then, to use AI-powered automation to address this challenge. Notable is continually (24/7/365) powering personalized digital outreach to patients and successfully enabling scheduling of tests and visits across a wide range of healthcare services. This gives patients power to schedule on their terms, and enables providers to trust their scheduling preferences will be respected.
Method
During 4 weeks in April 2023, Notable used an online platform to survey healthcare professionals working at health systems in a variety of patient access roles. Twenty-five executives and managers completed the survey.
Forty percent of the respondents were from hospitals or health systems. The remainder were from physician clinics, whether single or multi specialty organizations. 52% of the organizations included physicians of multiple specialities; 36% were specialty-specific institutions and 12% were exclusively primary care physicians.
Responses were unblinded.


Scheduling in health care remains a highly manual, telephone-based process
It’s hard to hire and retain enough people to do the work
52% of respondents report that it is the same difficulty to hire for call center talent as for other roles. 44% report that it is more difficult or worse.

Health systems have been reporting hiring challenges consistently since prior to COVID. Even entry-level positions are difficult to fill as hourly wages in other industries (e.g., retail, e-commerce) often exceed those at health systems. Turnover rates in health care are 4+ points higher than the average across industries and exceed commerce and shopping, education, and even food and beverage.
In spite of workforce challenges, scheduling hinges on humans making calls
The calls are repetitive, and since many go unanswered, they are not particularly rewarding — precisely the kind of work that can lead to burnout. Previous studies have shown that 57% of the healthcare workforce is personally worried about burning out due to repetitive tasks. Turnover in these roles is high as the past few years have led to what is commonly called The Great Reshuffle, with workers placing greater emphasis on compensation, company culture, and work-life balance.
64% of respondents report that more than 60% of their patient appointments are scheduled by telephone. Forty percent report that 80% of patient appointments are scheduled by telephone.

Existing processes are inefficient
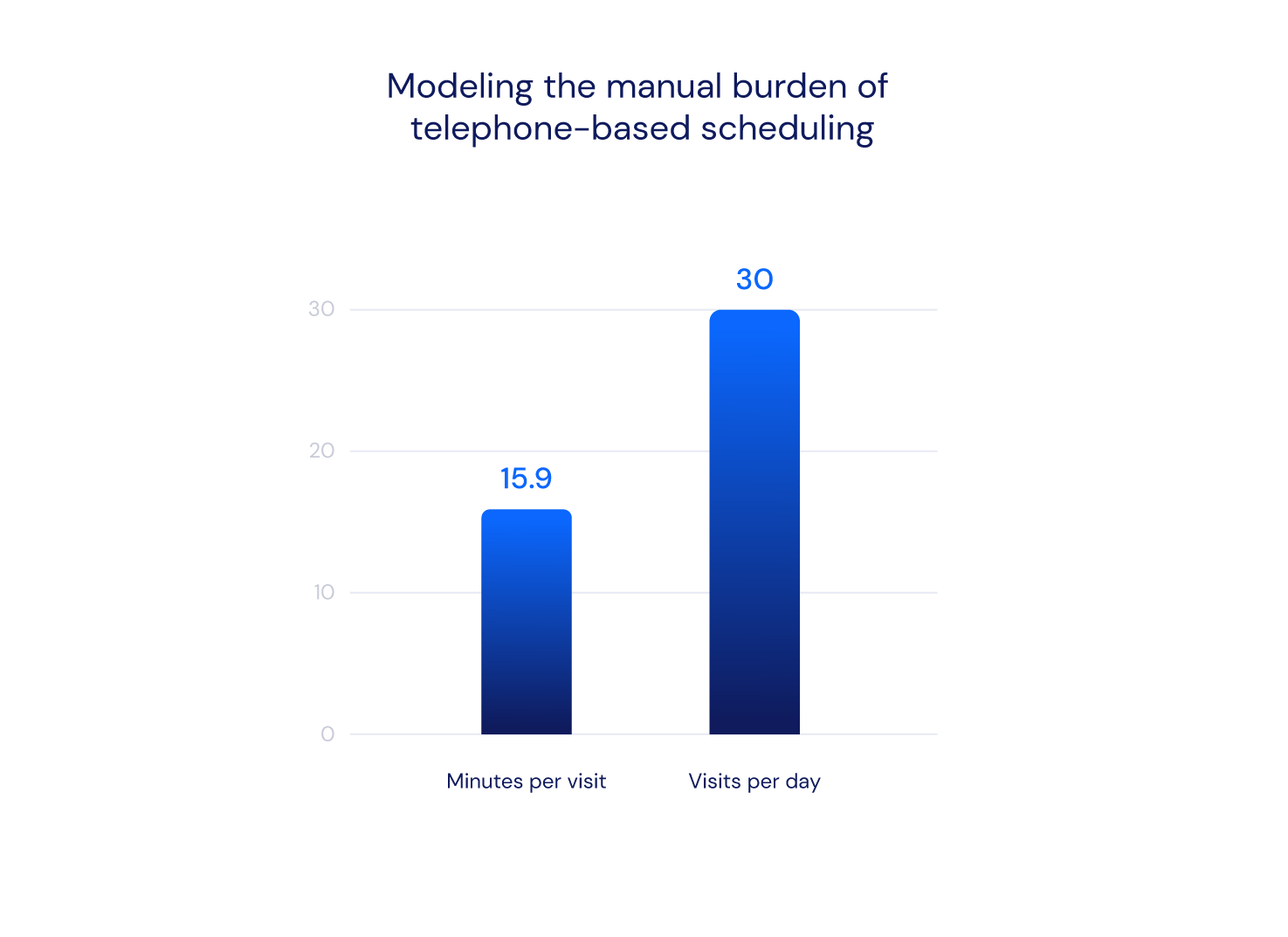
Organizations are almost evenly divided on the time spent per call - 52% report that it takes more than 6 minutes; 24% report that it takes 8+ minutes per call. The weighted average time per call reported was 6.9 minutes. Based on this data and NAHAM benchmarks, that means an average scheduler may only be able to schedule 160 total visits a week.

By contrast, automation can book thousands of appointments in minutes.
“We started to look at automating other solutions, particularly around COVID, when the vaccines became available,” said Todd Beardman, CMIO of North Kansas City Hospital and Meritas Health. “At one point we were booking 1,600 patients in 45 minutes. We could never have stood up a call center to be able to handle that kind of volume.”
Referral processing can double the time it takes to schedule a patient at a specialty center.
61% of respondents report that it takes 10+ minutes to process a referral. 22% of respondents report that it takes 16+ minutes. The weighted average reported processing time is 12.1 minutes.
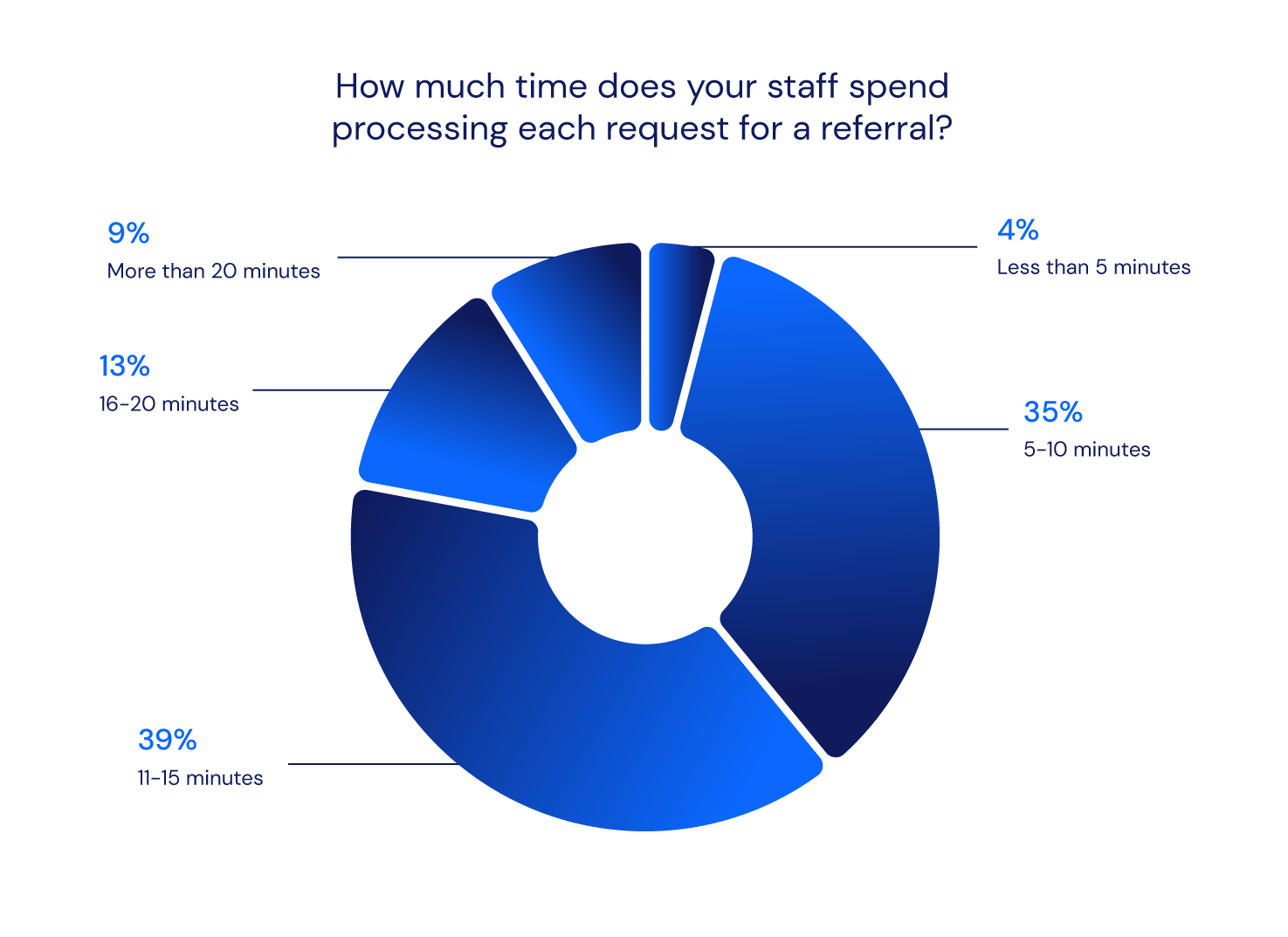
Depending on the physician specialty, from 20% to 70% of visits will originate from a referral. The American College of Cardiology reports that 80% of visits are initiated by a referral from a primary care physician. In otolaryngology, about 70% of visits result from referrals.. Processing referrals is a time intensive activity further adding to administrative and highly manual work. There is significant opportunity in this space for new revenue generation, but the manual burden can cause delays in scheduling patients efficiently for care.
Digital self-scheduling is urgently needed, but adoption lags
A mere fraction of appointments originate from digital self-scheduling
Digital scheduling is still nascent among providers. 71% of respondents report that less than 10% of visits are scheduled by patients online. 54% report that less than 5% of visits are scheduled by patients online. 13% of providers report that they do not offer patients self-scheduling online.

This despite the fact that patients want and expect to be able to self-schedule online. Last year’s survey showed that 70% of patients had tried to schedule a medical appointment online, but were ultimately redirected to a phone call to finish the process. And 61% of patients reported that hassles in the scheduling process can lead them to forgo care.
Providers are resistant to digital self-scheduling
The lack of digital self-scheduling in healthcare is due in large part to adoption resistance among providers. Nearly two-thirds of respondents report that less than half their providers even allow patients to self-schedule online into their calendar. 38% report that less than a quarter of providers allow patient self-scheduling online.

66% of respondents report that provider resistance stems from concerns about online scheduling systems capabilities. More than a third report that physicians have concerns that technologies won’t meet their needs; another 25% fear that technologies will not sufficiently prevent booking errors. Only 16% of respondents report that providers are not resistant to self-scheduling online.
EHRs still dominate the market
53% of respondents report that online scheduling is provided natively through the EHR.
47% of respondents report using a point solution.
While EHRs have served well as a system of record, using them as a system of action or intelligence has often led to unintended consequences. For example, EHR portal messaging has created an undue burden for providers struggling to manage the volume of patient messages. It should come as no surprise, then, that providers are reluctant to trust EHRs to manage direct access to their calendars.
EHRs lack the embedded intelligence to complete complex tasks without human intervention. Without the ability to easily adapt to clinician template preferences and patient needs, EHR-native digital scheduling may ultimately further complicate scheduling and require rework to fix any issues. This additional burden can be a source of major dissatisfaction for caregivers. A 2022 KLAS survey showed a strong correlation between EHR dissatisfaction and increased attrition risk.
Legacy scheduling tools get a passing grade, barely
We asked respondents to rate the performance of their current digital self-scheduling solution on a scale of excellent to terrible.
Not a single respondent rated the performance as excellent. 56% rated the performance of digital self-scheduling capabilities of current systems as good. The remainder — 44% — rated their performance as poor or worse.

Healthcare needs to move faster on automated, intelligent, self-serve scheduling
It’s time to hang up on phone-based scheduling
Scheduling serves as the gateway to health systems, determining ease of access. When patients are forced to call during business hours for appointments, it becomes challenging for working adults to access care. This presents an obstacle for an enormous percentage of the population who would have to take time from work to make a call — 76% of adults aged 25 to 54 work, and an increasing number of adults over 65 are remaining in the workforce. With only 19% of Americans picking up calls from unknown numbers, patients are also unlikely to receive incoming calls from their provider.
A 2022 Notable survey highlighted this frustration: 70% of patients had attempted online scheduling but were redirected to call to complete the process; 61% reported forgoing care due to scheduling difficulties. The demand for patient self-scheduling is evident.
Yet despite patient interest in self-scheduling, this survey confirms healthcare’s heavy reliance on telephone calls, even when that reliance is to its detriment. With 71% of executives admitting less than 10% of appointments are booked online, the bulk of healthcare scheduling is powered by human labor.
While scheduling calls average nearly seven (7) minutes each, that effort does not accurately reflect scheduler productivity. The National Association of Healthcare Access Management (NAHAM) benchmarks show that call preparation and documentation increase time spent considerably. For outbound calls, the patient answer rate, at best, is 33%. Taken together, this means that most schedulers likely calendar just 4-5 visits per hour, while the average physician scheduling queue ranges from 20-50 patients, depending on the specialty.
Considering the cost of staffing call centers and low answer rates, phone-based scheduling fails to deliver value and is an unsustainable model. It's time for a change.
Embracing AI-powered personalization for scheduling
While industries like travel, banking, bill payments, and investments have made significant strides in offering customers online services, healthcare has lagged behind.
82% of travelers book tickets online
61% of consumers use digital banking at least once a week
85% of consumers are already using digital bill pay
Despite the demand for digital scheduling in healthcare, adoption has been slow, primarily due to the underwhelming performance of legacy solutions. None of the surveyed executives considered their self-service experience excellent, with 44% rating it as poor or worse. Moreover, 63% of patients believe their provider's digital tools don't meet their expectations.
Legacy scheduling solutions fall short because they lack the intelligence necessary to adapt to each patient and clinician's needs. While EHRs serve effectively as a system of record, they were not designed to function as systems of engagement or intelligence. Provider resistance often stems from concerns about the inadequacy of online scheduling systems or their inability to meet specific needs. And even when digital scheduling is available, it typically only exists for inbound scheduling on the website — meaning patients have to initiate the process.
However, the intelligence to customize scheduling for every provider's preferences and personalize it for each patient's needs already exists. Every patient deserves access to intuitive, personalized digital scheduling. It also enables providers to be more proactive, reaching out to patients to schedule (outbound scheduling) instead of relying on the patient to remember when they should seek out care (inbound scheduling). AI enables true personalization at a scale that would be impossible with human labor alone, and is even potentially life-saving.
At Castell, care coordinators noticed Notable’s care gap automation surfaced that a patient was due for a colonoscopy at the three to five year interval instead of the usual ten. Notable automatically reminded the patient to schedule their colonoscopy, which ultimately revealed the patient had two pre-cancerous polyps that needed to be removed.
Patients and healthcare professionals are eager for technological advancements. Seventy-two percent of patients and 81% of healthcare professionals are hopeful that technology can improve their experiences.
It’s time to move beyond phone calls. Health systems already using AI capabilities have seen the benefits.
“By investing in intelligent automation, we are removing the burden on the patient to determine when they need to be seen for care,” said Kristen Guillaume, CIO of North Kansas City Hospital & Meritas Health. “At the same time, we are enabling the provider to take a more proactive approach with each patient.”
AI-powered personalization can deliver superior results more cost-effectively. Examples include:
- A scheduling system that remembers the patient and pre-populates their information
- A scheduling system that proactively notifies patients when they are due for preventive screenings
- A scheduling system that collects required patient information before the appointment and alerts the patient if their insurance card is invalid
- A scheduling system that provides appointment cost estimates and suggests payment plans based on the patient's history
- A scheduling system that leaves an actionable digital footprint which the patient can engage with when they are ready to do so.
Notable is leveraging artificial intelligence and automation to solve these very challenges. We are working with health systems nationwide to combine personalized digital outreach with direct online scheduling to meet the needs of both patients and administrative staff.
Visit notablehealth.com to learn more.








.png)